Why is early diagnosis of Dementia important?

Early diagnosis of dementia is essential! Most are unaware that dementia is treatable, by ‘treatable’ I do not mean curable but we can with expert help maintain an individual’s brain […]
Jonathan’s Dementia Conference speech: Non-pharmacological Interventions

Re-defining the Dementia Pathway Written by Jonathan Hanbury, Clinical Director & CEO of The Ness Care Group, for the UK Dementia & Palliative Care Conference. I feel I should very […]
Press Release
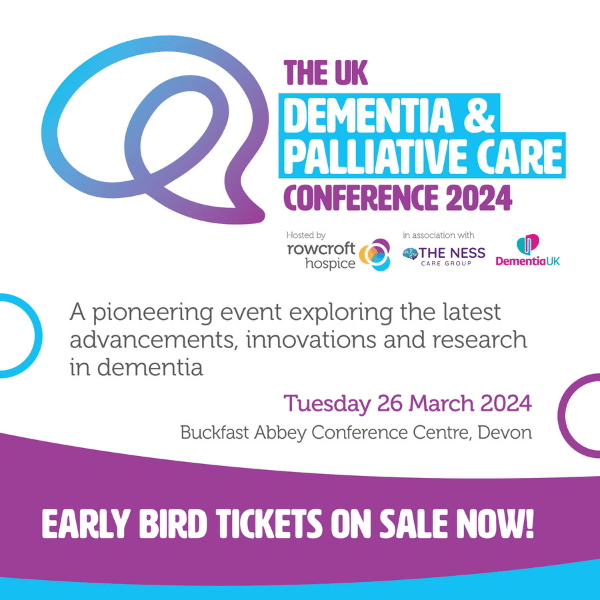
Rowcroft and The Ness Care Group unveil groundbreaking Dementia and Palliative Care Conference in the South West Rowcroft Hospice is thrilled to unveil its plans to host a Dementia and […]
The Future for Dementia in an Ageing Society

Last month our Chief Medical Officer published the annual report in to Health in an Ageing Society. The report is a stark reminder that the UK is an ageing society […]
Part 2 Compassionate Communication

In part 1 on compassionate communication, I spoke about the impact of verbal, non-verbal and the external environment on communication. I picked out 4 tips for improving communication: Recognise that […]
Part 1 Compassionate Communication

In this blog we explore what it means to communicate well with someone living with dementia. What you can do to ensure compassionate enabling communication. It is a topic close […]
Q&A with… Cora Wilkie

How did you get involved in dementia care? As a social psychologist I have always been interested in Ageing. I find it a challenging stage in life and I admire […]
Q&A with… Kate Bath

We caught up with our Specialist Coach, Kate Bath to ask her a quick fire Q&A… How did you get involved in dementia care? I originally got into Dementia care […]
Q&A with… Jade Barlow

We sat down with our Manager & Specialist Coach, Jade Barlow for a quick tea break and asked her some questions about working for Atlas, her dementia experience and her […]
Technology in Dementia

For many years I have been sceptical about the potential of technology in cognitive decline. Not against it but sceptical and I must admit a little frustrated that a lot […]
